In the hospital, routines carry us through our days and lend a semblance of structure to the chaos of lives disrupted by illness. Some routines happen on a large scale—weekly gatherings of departments for Grand Rounds, hospital leadership meetings for safety huddles, the hustle of getting a cadre of operating rooms started nearly simultaneously in the predawn. Other routines are more intimate—the sequenced process of doing a sterile central line dressing change, the donning and doffing of PPE outside a patient’s room, the one-one-one nursing handoff at shift change.
Read moreStill We Dream: How We Face the Unpredictable World by Mary Anne Moisan
Humans can create a world through perception, imagine a potential life, whether it be the life of a relationship or the life of a baby. We fill in the unknown details to make a whole that is pleasing and good. It’s as if we willfully ignore that so much of life is unpredictable.
Read moreWhen the “Clock of the Living” Runs Down: A Reflection by clinical social worker and chaplain Betty Morningstar
The fractured stories at the end of life often reflect an ineffable but powerful experience of creativity, insight or even revelation. These opportunities arise because the dying person doesn’t see time according to the clock of the living. Imagine how much one could conceive of were time not of the essence.
Read moreThe Limits of Love: A Reflection by Carmela McIntire about Anorexia, Overeating and Fulfillment
Disordered eating occupies a spectrum—anorexia nervosa at one end, morbid obesity at the other. Attempting rigid control of the body and its appetites, anorexics are unable to see themselves and their bodies accurately. Compulsive overeaters—often obese—similarly might not see themselves accurately. In both disorders, controlling food is the aim, a genuine addiction, a strategy through which addicts deal with the world and their own circumstances—a necessary coping skill, even though it is risky to health in both cases.
Read moreWhat I Learned about the ICU: A Reflection by Benjamin Rattray
In her essay “The Shape of the Shore” (Spring 2020 Intima), Rana Awdish takes us into the intensive care unit during the ravages of a pandemic. She shows us “…the desperate thrashing patients on the other side of the glass” and “…the sticky blood on the floor.” As I read the words, my breath becomes shallow as fear and grief pummel into me. Somewhere deep, beneath the shrouds of consciousness, the words resonate, and I feel as though I am slipping beneath an indigo sea.
Read moreMothers and Daughters: A Reflection on Cancer, Caring and Seeing the Whole Picture by poet Kathryn Paul
—After ‘Macroscopic” by Adela Wu (Spring 2021 Intima)
My mother and I were not close. I knew she wanted us to be, but I couldn’t do it her way. For most of my adult life, I kept my distance, emotionally and physically. We lived on opposite sides of the continent. In her 80’s, the creeping dementia my mother never discussed was overtaken by a cruel and much more terrifying diagnosis: Stage IV ovarian cancer.
Aided by her cancer-free twin sister, Mom endured multiple surgeries and two lengthy and debilitating rounds of chemo. Each time, her cancer came roaring back within weeks. Her surgeon suggested an experimental Round Three. Mercifully, her oncologist suggested hospice at home instead.
During the first year of Mom’s illness, I was trapped by my own cancer treatment, unable to participate in her care. I called daily, spoke with her, spoke with my aunt, asked about her pain, her “tummy trouble,” her ascites, and her white count. I took notes and dictated the questions to ask at her next appointment.
As soon as my doctors cleared me to visit her, I did. I was always on the verge of moving in with her, but never quite needed to do so. I flew back and forth. The more debilitated she became—by her cancer and her dementia—the more often I visited.
Adela Wu’s Studio Art piece “Macroscopic” simply and eloquently captures the changes in how I experienced my mother during those last months and weeks. The simplest things gave her joy: A small dish of ice cream. A pain-free nap on the down-stuffed cushions of her couch. Cuddles with her cats. A bird visiting the feeder outside her window.
Even as her disease spread through her body, even as she faded, my mom seemed to crystallize. She became, ultimately, the Essence of herself. And—just at the end—I finally saw her.
Kathryn Paul
Photo by Andrew Givhan
Kathryn Paul (Kathy) is a survivor of many things, including cancer and downsizing. Her poems have appeared in Rogue Agent, Hospital Drive, The Ekphrastic Review, Lunch Ticket, Stirring: A Literary Collection, Pictures of Poets and Poets Unite! The LiTFUSE @10 Anthology. Her poem “Dementia Waltz” appears in the Spring 2021 Intima.
Shakespeare, Stanzas and How We Think About Death by Albert Howard Carter, III, PhD
When my sonnet “All Tuned Up” appeared (Spring 2021 Intima), I was asked to write about another piece published in the journal. I chose “I Picture You Here, But You’re There” (Spring 2020 Intima) by Delilah Leibowitz. Her poem and mine both explore how we think and feel about death.
Read moreHow Touch Affects Healing, a reflection by Wendy Tong
In her Field Notes essay “Hand Holding” (Fall 2019 Intima), Dr. Amanda Swain describes the experience of beginning her surgery rotation as a third year medical student. In the early days of the rotation, she feels an intense sense of being out of place within the “intricately choreographed dance” of the operating room. But when the next patient is wheeled in, Dr. Swain is reminded of how a nurse once took her hand before she underwent surgery, the touch conveying an unforgettable message of comfort during a time of deep vulnerability.
Read moreReimagining Chaos in Art and Poetry by Selene Frost
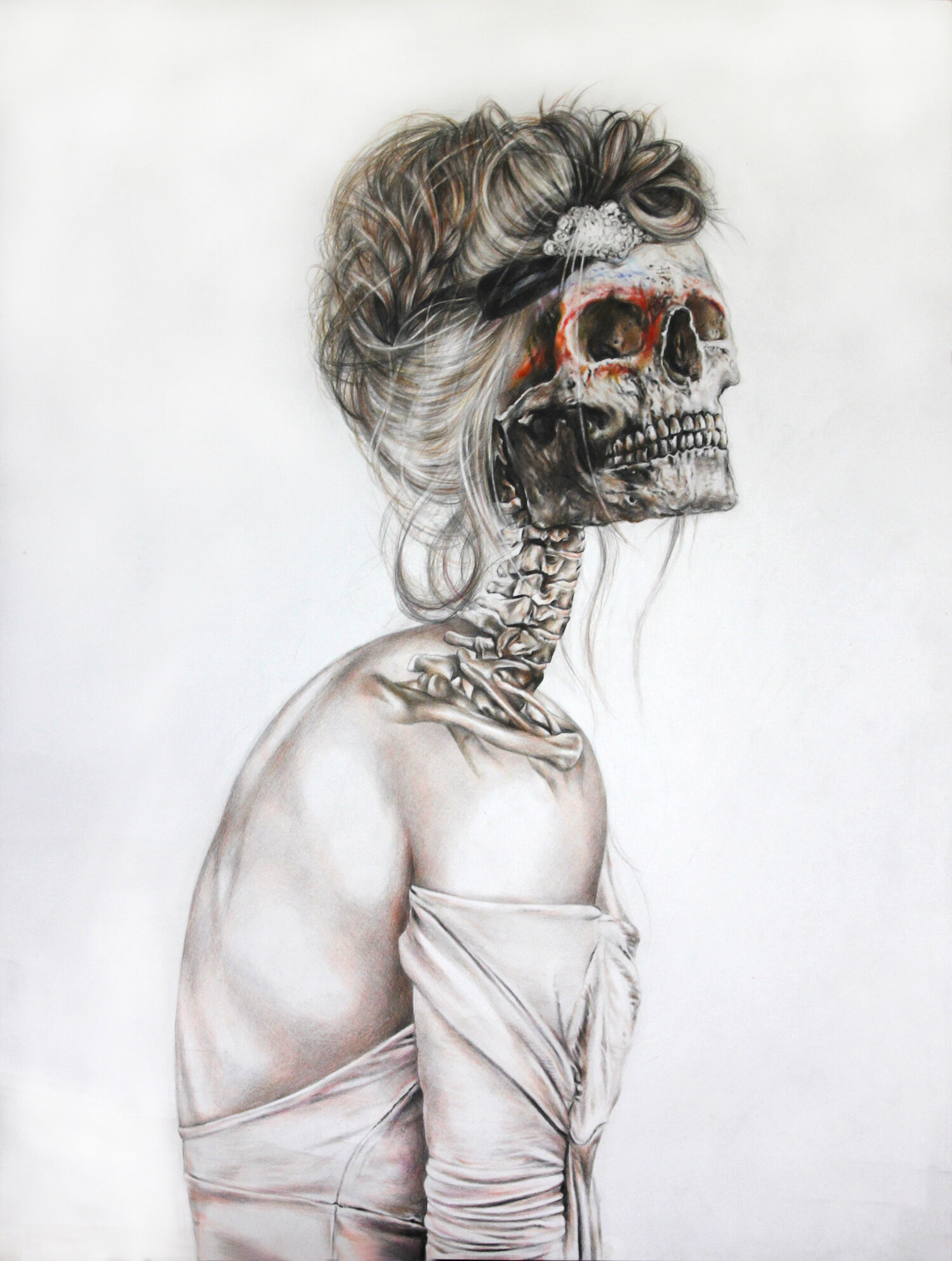
Anatomy of the Vogue by Meagan Wu. Fall 2017 Intima: A Journal of Narrative Medicine
I’ve long been fascinated by the way structure informs poetics and the practice (and in this case—reception of medical care). In my piece “Field Notes on Form,” I extol the ways in which linguistic structure has the remarkable ability to organize our thoughts, increase our signal within the noise, and etherealize the mundane. In “Post NICU Villanelle,” Joyelle McSweeney uses language not only to remediate the chaos of loss and of leaving but also to deconstruct both the poetic form and herself.
Read moreLife in the Gaps: How Illness Transforms Our Sense of Time by Renata Louwers
It was in those gaps, between our lived experience—the crushing uncertainty about how long my husband would live, the daily reality of his intolerable pain, and the abrupt shift from a life of joyful ease to one spent contemplating death—and the oncology profession’s standards of care, first-line treatments, and numeric pain scales that my frustration festered.
Read moreBecoming the Superheroes Our Parents Need: The Journey from Child to Worthy Caretaker by Usman Hameedi
Our parents are often our first examples of superheroes. They make gourmet meals from minimum wage, give hugs that vanquish our demons, and provide limitless love. They are impervious to damage or decay and are always ready to save our days. So, seeing the human in them, the mortality in their breath is unsettling. When they come to need us, we feel so grossly unprepared.
Read moreWhat Does ‘Paying Attention’ Mean in a Healthcare Setting? A Reflection by Ewan Bowlby
Ewan Bowlby is a doctoral student at the Institute for Theology, Imagination and the Arts (ITIA) in St Andrews. He is researching ways of using mass-media artworks to design new arts-based interventions providing emotional, psychological and spiritual care for cancer patients. Bowlby’s paper “Talk to me like I was a person you loved”: Including Patients’ Perspectives in Cinemeducation” appears in the Spring 2021 Intima: A Journal of Narrative Medicine.
Narrative Medicine is about creating connections: finding words, ideas or stories that bridge the gap between patients and health professionals. This search for common ground is beautifully rendered in Carol Scott-Conner’s short story “Christmas Rose” (Spring 2017 Intima). Her fictional narrative reveals how mutual understanding can emerge in unexpected places. An encounter between the resolute, inscrutable Mrs. Helversen and her oncologist shows that the relationship between a physician and patient can flourish when the physician pays attention to the intimate, personal details of a patient’s story.
Initially, the clinical encounter in “Christmas Rose” seems unpromising, hampered by reticence and disagreement. Mrs. Helversen, who has a neglected tumor on her breast, has been “strong-armed” into a cancer clinic by her concerned daughter, and she is not receptive to the prospect of treatment. Scott-Conner, a Professor Emeritus of Surgery at the University of Iowa Carver College of Medicine, switches the first-person narrative from Mrs. Helversen to her oncologist, allowing the reader to inhabit two alternative perspectives on the same meeting and reminding us that the same interaction can be interpreted very differently.
When I wrote an academic article that appears in the Spring 2021 Intima proposing that patients’ perspectives should be included in “cinemeducation,” these differences in interpretation were central to my argument. Showing clips from films to encourage medical students to relate to a fictional patient is an excellent idea. Yet listening to how patients respond to these clips can enrich this pedagogical method. As I demonstrate through the qualitative research presented in my article, patients “see things differently.” The same fictional scene featuring a patient-doctor interaction can draw responses from patients that surprise and challenge healthcare professionals. So, why not use such scenes as a space in which different perspectives can be expressed and discussed, bringing patients and providers together through the audio-visual medium?
In “Christmas Rose,” it is a rock that facilitates this meeting of minds. While the oncologist is surprised when Mrs. Helversen describes her tumor as a “rose,” betraying a complex emotional attachment to the growth, she finds a way to react empathetically and imaginatively to Mrs. Helversen’s unusual behavior. Offering the elderly patient a desert rose rock in exchange for her tumorous “rose,” the oncologist persuades Mrs. Helversen to accept treatment. This fictional oncologist shows an adaptability and ingenuity that the health professionals involved in my research also exhibited. In my article, I describe how health professionals engaged constructively with patient’s unique or unexpected responses to imagined patient-doctor interactions in films. Listening to both sides and hearing alternative perspectives on the same encounter can yield important, enlightening insights, whether one is participating in a focus group, watching film clips or doing a close reading of a short story such as “Christmas Rose.”
Ewan Bowlby is a doctoral student at the Institute for Theology, Imagination and the Arts (ITIA) in St Andrews. He is researching ways of using mass-media artworks to design new arts-based interventions providing emotional, psychological and spiritual care for cancer patients. This involves using fictional narratives, characters, and imagery to reflect and reframe patients' experiences of living with cancer, helping them to understand and articulate the effect of cancer on their lives. He is developing the impact of his research through an ongoing collaboration with Maggie Jencks Cancer Care Trust (Maggie's) and Northumberland Cancer Support Group (NCSG). Other interests include theological engagement with popular culture, the relationship between theology and humor and the use of narrative form for theological expression. Bowlby’s paper “Talk to me like I was a person you loved”: Including Patients’ Perspectives in Cinemeducation” appears in the Spring 2021 Intima: A Journal of Narrative Medicine.
Giving: What Real Generosity Looks Like in Healthcare by pediatrician Lane Robson
Giving defines us as individuals. Patients and healthcare professionals are obliged to share time together. Gifts of shared humanity transcend personal and professional obligations. These gifts might be hoped for but are neither expected nor routine.
Thresholds and Transgressions, a reflection on ICU chaos, communitas, liminality and Levinas by Nancy Smith
Nancy Smith is a retired Registered Nurse. Though she moved through the many domains of hospital nursing, most of her work took place in an Intensive Care Unit. Her co-workers noticed that she would place small strips of paper with poems by various authors on her locker from time to time along with the pictures of her family.
Read moreOn Trauma, Hope and Dragonslayers, an essay by hospital-based physical therapist Galen Schram
Can what we know about PTSD in frontline workers who treated the victims of the Boston Marathon bombings help us understand how to care for our COVID-19 frontline workers? What will be done to understand and treat race-based traumatic stress, a term I hadn’t heard until this summer?
Read moreThe Practice of Prolonging Death, a reflection by palliative care physician Chris Schifeling
“Would we rather die too soon or too late?”
The taboo of talking about death combined with a faith in the insomnia of medical technology leads many to err far on the side of dying too late.
Read moreAre We Still Ourselves? By Marie-Elisabeth Lei Holm
Facing death led Kalanithi to grasp the flow of time in an entirely different way. From being a steady currency–a predictable resource of skill-building and career advancement–it dawned on him that time does not always follow a linear path of progress.
Read more“A Line Blurring Joy and Grief”: Empathizing from a Distance, by Daniel Ginsburg
How do clinicians carry on their vital work without bearing the grief of patients and their families, yet still comfort them?
Read moreCaught between Floating and Drowning, a reflection about poetry, memory and adapting to chaos by Mikayla Brockmeyer
A state of flux. The COVID-19 pandemic has induced a state of “How will I react to _____?” Listlessness and emotional exhaustion bring about feelings of isolation and longing to be somewhere we are not. Yet, in learning to modify behaviors, collaborations have emerged.
In the opening couplet to Sheila Kelly’s poem entitled “Breathe” (Fall 2017 Intima). she sets the stage and introduces a poignant metaphor, depicting calmness, yet incertitude.
You are floating in the swimming pool again.
Your childhood best friend rises like prayer.
“Breathe” was penned well before the current pandemic, yet the feelings of serenity and safety one day, and panic the next, expressed are relevant today. Using a second-person narrative, she paints a vivid picture of a disjointed home life, sifting through old, painful memories. In the poem, the main character is catapulting between chaos and “floating in the swimming pool.” At the end, I interpret a sense of adaptation from the character that leaves a residue of hope.
In my essay “Turbulent Undertow” (Fall 2020 Intima), parallel feelings are grappled with, as I describe a surfing attempt, and later, my experience as a hospitalist scribe. Woven together, I write about two near-drowning experiences: on surfing and on caring for patients with COVID-19. The best friend in Sheila Kelly’s poem encourages the main character to put on her old swimsuit when distressed. After a long series of days working with the hospitalist, I, too, wanted to offer solace. But instead, all I could offer was “Glad you’re okay,” a phrase that has reverberated through my brain ever since I first heard it myself.
Riding metaphorical surfboards together and finding ways to float in metaphorical swimming pools may not be the best solution to curb the emotional toll of the pandemic. However, validation and shared human connection serve as two ways to avoid possible drowning amidst the pandemic waves.
Mikayla Brockmeyer
Mikayla Brockmeyer is a first year osteopathic medical student at Des Moines University in Des Moines, Iowa. She began working as a hospitalist scribe in 2018, while she was enrolled in the Master of Science in Biomedical Sciences program at Des Moines University. She successfully defended her thesis in 2019 and spent her gap year scribing full time. This is her first time showcasing her storytelling abilities in a public arena. Her non-fiction essay “Turbulent Undertow” appears in the Fall 2020 Intima.
‘Differential Diagnosis’ Can Be A Lifesaver, a Reflection by Colleen Corcoran
© Differential Diagnosis by Yan Emily Yuan Spring 2020 Intima A Journal of Narrative Medicine
Accurate differential diagnosis can save a life. By being able to determine clearly how one outlying factor or the combination of a group of signs and symptoms tips the scale to the correct pattern confirmation and treatment, our lives can be shaped, saved and lost in this qualifying lens of time. It’s integral to the practice of medicine, but also in many ways to how we make decisions in life. A positive or negative result, a clustering of symptoms, the ticked boxes and specimen samples that can reveal so much as to how we define our experiences of life and are able to move forward.
Read more